Blood Test’s Correlation with Rapid Cognitive Decline in Alzheimer’s Patients: A Study at the European Academy of Neurology
Blood Test’s Correlation with Rapid Cognitive Decline in Alzheimer’s Patients: A Study at the European Academy of Neurology
A study presented at the European Academy of Neurology (EAN) Congress 2025 in Helsinki, Finland, investigated the correlation between insulin resistance and the rate of cognitive decline in Alzheimer’s disease patients. Researchers from the University of Brescia’s Brain Health Center in Italy analyzed data from 315 non-diabetic patients with cognitive decline, including 200 with confirmed Alzheimer’s disease and 115 with other neurodegenerative disorders. The study utilized the triglyceride-glucose (TyG) index, a common blood test assessing insulin resistance, as a key metric.
Participants underwent the TyG index blood test and were followed for three years. The study focused on a subgroup of 161 patients with mild cognitive impairment due to Alzheimer’s disease. Researchers divided patients into tertiles based on their TyG index. Results showed that Alzheimer’s patients in the highest TyG tertile (indicating the highest level of insulin resistance) had a significantly increased risk of faster cognitive decline compared to those in the lowest tertile. Specifically, they were over four times more likely to experience a decline of more than 2.5 points per year on the Mini-Mental State Examination (MMSE), a widely used cognitive function assessment tool (hazard ratio: 4.08; 95% CI: 1.06–15.73).
This association between high TyG index and rapid cognitive decline was not observed in the group of patients with other neurodegenerative diseases. Further analysis revealed that high TyG levels in Alzheimer’s patients were linked to increased cardiovascular risk factors and markers of blood-brain barrier disruption. However, no interaction was found between high TyG levels and the APOE ε4 genotype, a known genetic risk factor for Alzheimer’s disease, suggesting that metabolic and genetic risks may operate through distinct pathways.
Lead investigator Dr. Bianca Gumina noted that the findings were unexpected, as the effect was specific to Alzheimer’s disease and not observed in other neurodegenerative conditions. She highlighted the potential for the TyG index to identify Alzheimer’s patients at higher risk of rapid cognitive decline, enabling more targeted interventions and potentially influencing the selection of patients for clinical trials of disease-modifying treatments. The researchers suggested that insulin resistance might contribute to faster cognitive decline by impairing brain glucose uptake, promoting amyloid buildup, disrupting the blood-brain barrier, and fueling inflammation.
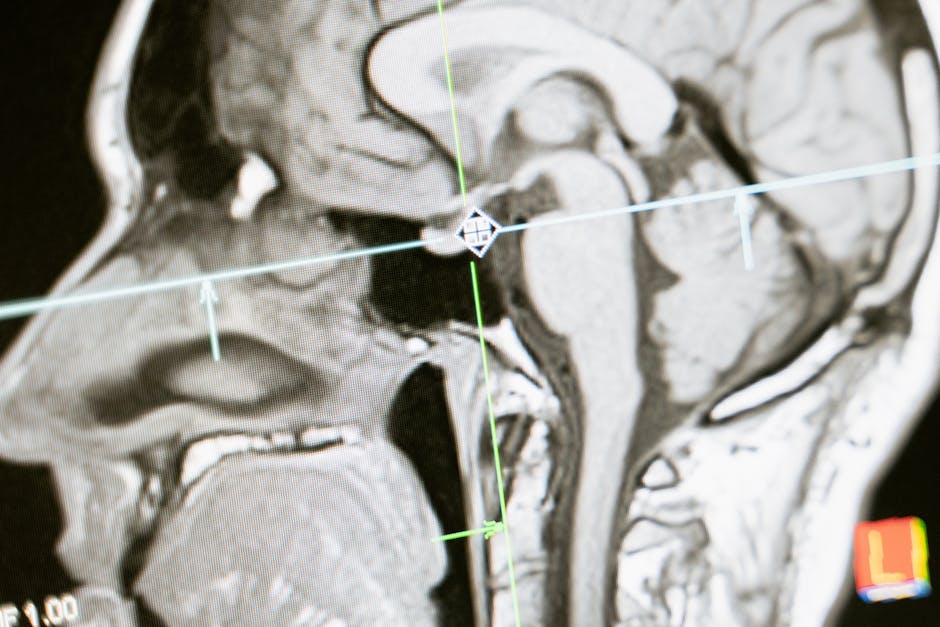
The study also mentioned ongoing research to investigate whether TyG levels correlate with neuroimaging biomarkers of Alzheimer’s disease. The potential integration of TyG index results with neuroimaging data could improve early detection and allow for a more personalized approach to Alzheimer’s disease management. Dr. Gumina emphasized the potential for targeting metabolism as a readily modifiable factor in delaying disease progression, potentially working alongside emerging disease-modifying drugs.
It is important to note that the findings presented at the EAN meeting are preliminary and have not yet been published in a peer-reviewed journal. The research involved a retrospective, single-center study, limiting the generalizability of the findings. Further research is needed to validate these results in larger, more diverse populations and to explore the clinical implications of using the TyG index for predicting disease progression and guiding treatment strategies.
Disclaimer: This content is aggregated from public sources online. Please verify information independently. If you believe your rights have been infringed, contact us for removal.